Sleep Apnea
Sleep Apnea
Sleep apnea is a common and under-diagnosed disorder that can significantly impact the quality and quantity of one’s sleep.
What is Sleep Apnea?
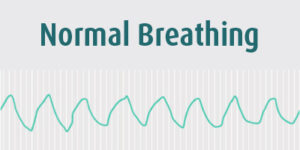
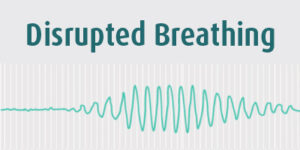
Sleep apnea is a breathing-related sleep disorder characterized by repeated disruptions in normal breathing that can last anywhere from a few seconds to over a minute. In most cases, the pauses in breathing are caused by an obstruction of the airway. The blocked airway may result in a loud snort or gasp that wakes the patient up, disrupting sleep. Depending on the length and frequency of an episode, the sufferer may experience substantial oxygen deprivation.
Types of Sleep Apnea
Sleep apnea is usually classed as either obstructive sleep apnea (OSA) or central sleep apnea (CSA). The classification is determined by the dominant type of event.1Often people with sleep apnea have some combination of both obstructive and central events.
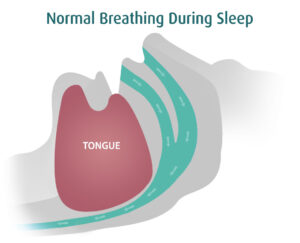
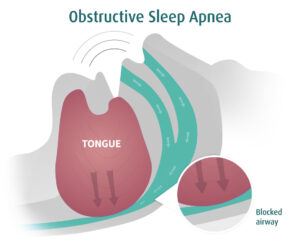
Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea occurs when a person experiences a partial or complete blockage of the airway during sleep. The obstruction can be due to bodily features or to a relaxation of the muscles in the chest and neck during sleep.This is the most common type of sleep apnea. The severity of OSA is rated according to the number of breathing events per hour of sleep:
- $Mild OSA – 5-15 episodes per hour of sleep
- $Moderate OSA – 15-30 episodes per hour of sleep
- $Severe OSA – 30+ episodes per hour of sleep
OSA Can Kill
Left untreated, OSA is associated with increased mortality risk and comorbidities, including cardiovascular diseases, depression, and stroke.
Central Sleep Apnea (CSA)
Central sleep apnea (CSA) occurs when the brain fails to signal the breathing muscle (diaphragm) to activate. As a result, the sleeper either “forgets” to breathe or breathes less deeply than normal.3Notably, “pure” central sleep apnea (no obstructive events) is uncommon. Central sleep apnea generally refers to patients who have more central events than obstructive events.
What is Central Sleep Apnea
Central sleep apnea is defined as “the temporary withdrawal of central (brainstem-driven) respiratory drive that results in the cessation of respiratory muscle activity and airflow.” To better understand this definition, it is helpful to compare central sleep apnea with normal breathing. In a healthy person, the brain signals the breathing muscle (diaphragm) to contract at regular intervals. The signal to breathe travels from the brain stem down the phrenic nerve to the diaphragm, causing a contraction. This contraction of the diaphragm pulls air into the lungs. In persons with central sleep apnea, the brain fails to send regular signals to the diaphragm. The result is an extended “pause” of breathing, lasting roughly 10 to 40 seconds. An episode may result in:
- $Sleep disturbance
- $Decrease in the body’s oxygen levels (also known as hypoxia)
- $Surge of norepinephrine (the body’s “fight or flight response,” which may feel like a racing heartbeat).
These events can happen multiple times an hour—sometimes as frequently as once per minute. However, these sleep disturbances are often not enough to fully wake the person. The sleep partner may actually be more likely to identify the breathing disorder than the person themself!
Symptoms of Untreated Central Sleep Apnea
Central sleep apnea has both long term and short term symptoms:
- Chronic fatigue
- Excessive daytime sleepiness
- Brain fog / cognitive impairment
- Inability to fall asleep or get restful sleep
Many patients with CSA also have heart disease, especially heart failure. Within this population, patients with CSA are at increased risk for hospitalization and even death.
Central Sleep Apnea Causes and Associations
Central sleep apnea is caused by the failure of the brain to consistently send signals to activate the breathing muscles while asleep. Central sleep apnea has a number of known associations, including
- Cardiac disorders, including congestive heart failure (CHF) and atrial fibrillation (AFib)
- High altitude
- Opioids
- Treatment emergent central sleep apnea
- Idiopathic central sleep apnea
- Other medical conditions (e.g. stroke, brainstem/spinal cord disorders)
CARDIAC DISORDERS
Studies have shown that up to 40% of people with congestive heart failure (CHF) and 30% of people with atrial fibrillation (AFib) may have central sleep apnea. In fact, heart failure is the most common cause of CSA in the general population.2
HIGH ALTITUDE
Periodic breathing occurs when people are exposed to high altitudes. This may be due to the way the body responds to changes in the atmosphere.
OPIOIDS
Certain medications, including opioids, can disrupt breathing patterns and lead to central sleep apnea.
(CSA) Include:
Mixed Sleep Apnea (MSA)
Other classifications of sleep apnea may also be used. Mixed apnea refers to events that are both central and obstructive in nature. Typically, the apnea will begin as a central sleep apnea and then an airway obstruction follows.Complex apnea typically refers to central events that arise only after positive airway pressure (PAP) therapy is applied.
What Is Upper Airway Resistance Syndrome (UARS)?
Upper airway resistance syndrome is a precursor to obstructive sleep apnea. It is important to identify and treat patients with UARS since they have a higher risk of developing obstructive sleep apnea in the future. It is commonly believed that sleep apnea begins as this sort of subtle airway collapse (which may or may not be associated with snoring). On its own, upper airway resistance syndrome can have a harmful effect on an individual’s health and sleep quality due to chronically disrupted sleep.
What Is Upper Airway Resistance Syndrome (UARS)?
Upper airway resistance syndrome is a precursor to obstructive sleep apnea. It is important to identify and treat patients with UARS since they have a higher risk of developing obstructive sleep apnea in the future. It is commonly believed that sleep apnea begins as this sort of subtle airway collapse (which may or may not be associated with snoring). On its own, upper airway resistance syndrome can have a harmful effect on an individual’s health and sleep quality due to chronically disrupted sleep.
Symptoms of Sleep Apnea & Upper Airway Resistance Syndrome
Symptoms of sleep apnea and UARS vary from person to person. These symptoms can include:
- Loud snoring
- Choking or gasping during sleep
- Frequent waking throughout the night
- Excessive daytime sleepiness
- Unrefreshing sleep
- Morning headaches
- Memory loss
- Trouble concentrating during the day
- Irritability
- Depression
- Mood swings
- Dry mouth or sore throat when waking up
If you are experiencing any of these symptoms, schedule an appointment with our sleep specialists for sleep apnea/UARS diagnosis and treatment.
Risk Factors for Developing Obstructive Sleep Apnea & UARS
You may be more likely to develop sleep apnea or upper airway resistance syndrome if you have one or more of the following pre-existing conditions:
- Overweight / obesity
- Narrow airway
- Nasal congestion
- Neck circumference greater than 43 cm
Other risk factors may also include:
- Age
- Gender
- Family history of sleep apnea or UARS
- Smoking
Types of Sleep Disorders
Sleep Apnea
Narcolepsy
Insomnia
Restless Legs Syndrome (RLS)
Parasomnias
Pediatric Sleep Disorders
Circadian Rhythm Disorders
Other Sleep Disorders
Title
Title
Explore Treatment Options
Book a session with one of our advisors to learn more about the next steps and we will get in touch with you shortly.
Need More Information?
Could not find answers to your questions? Get in touch with one of our advisors to learn more about your sleep disorder and we will get in touch with you shortly.
